Doctor Fighting on the Front Lines Reveals How a ‘Tiny Breathing Tube’ Separates Life and Death for Patients
Like many medical practitioners around the country, Dr. Jason Chiu is sacrificing his health by dedicating his time and energy towards fighting the COVID-19 crisis head-on.
Chiu, who is an anesthesiologist and founder of his private practice, The Painless Center, dedicates two to three days out of his week to work 12-hour shifts at major hospitals in New York and New Jersey. He works on what is called the “special intubation unit,” a team composed of him and three other colleagues.
Chiu’s job is to intubate or insert breathing tubes into patients suffering from complications due to COVID-19. Since the process of intubation is very specialized, Chiu told NextShark that he feels the responsibility to step up as someone who has the proper skillset.
“This is really a defining history in time,” he added. “It is time to step up because if I am lucky to have the ability to do what I do as an anesthesiologist, I realized at this time that I can really apply my skills.”
On an average day, Chiu completes 7-10 intubations on critical care patients who are typically in the 55-70 age range. However, he has had several cases involving people in their 20s with no underlying conditions. On March 24, he shared on Facebook that he had to intubate a COVID-19 patient who, only four days before, walked into the hospital as a relatively healthy young adult.
“Now his entire life depends on just a tiny breathing tube,” he wrote.
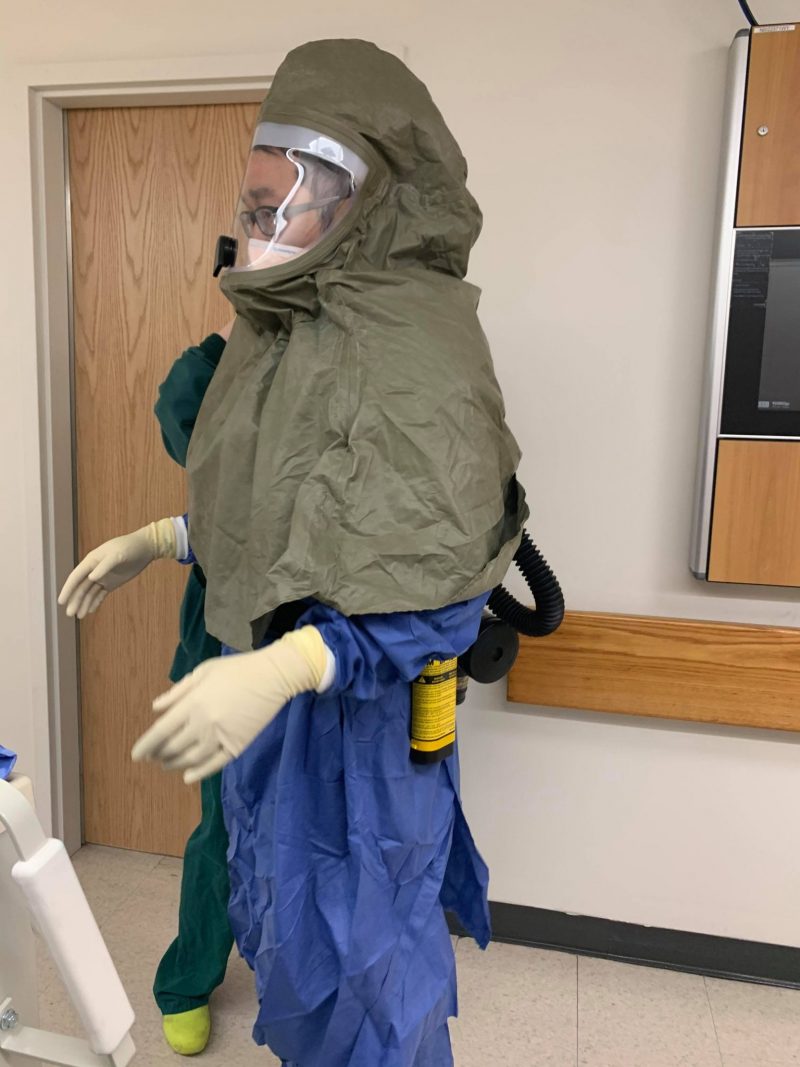
Anesthesiologists are more at risk of contracting the virus due to the nature of their job. When intubating a patient, they have to open up the airway which exposes them to aerosols and viral particles. Therefore, they are usually allocated more PPE (personal protective equipment). Chiu’s “purified air power system” takes five minutes to put on and is the same protective gear used in chemical warfare, as it filters viral particles.
Besides the lack of PPE in hospitals, the improper utilization of the gear has also been an issue. The masks that Chiu wears need to be fit tested or tailored to the contours of the doctor’s face. He says this process is currently not being done, subjecting health care practitioners to more risk. Chiu is down to only two people per shift on his team after some of his colleagues caught the virus. There are typically about three people per shift.
Another issue front-liners face is keeping their mental health in check.
“Mentally, it is exhausting,” Chiu said. “I am constantly worried, ‘am I catching this virus?’ You are constantly under this surveillance, it’s a little bit of paranoia that’s mentally draining.”
“You either become really depressed, very fearful, where you go into a mode of hysteria,” he continued.
Chiu says he finds different mechanisms to cope and “try to have a positive attitude about it.”
It can also be emotionally taxing because of what he witnesses at work all day.
“A lot of these patients that we intubate, not to be pessimistic… many don’t come out of it alive,” Chiu said. “It is daunting knowing that my face, my gear, this is the last thing they see.”
As a father of a six-month-old baby girl, he faces constant decisions. Chiu says it is difficult leaving his “family and being able to tell them ‘hey, you don’t know if this is the last time I can see you before I catch something” and wondering, “Should I leave my family somewhere else?”

Chiu called attention to healthcare workers not receiving financial and political support that would be expected during a pandemic. The resources necessary for the job are simply not being provided which is frustrating for Chiu.
“Instead of having support, most healthcare industries are cutting staff because these healthcare companies are not generating what they were used to generating,” he said, adding that some of the staff in his group are being placed on furlough.
Chiu encourages people to “look at the hospital as a whole.” The clinic staff and nursing aides “are in the same unit, they have the same exposure, they are cleaning these units and they are often overlooked.”
There has also been a spate of xenophobia and racism as a result of the outbreak.
“I think it is very unfortunate that Asian Americans are being targeted for this whole situation based on just an instance in Wuhan,” Chius said. “Chinese people are struggling too. If I am a Chinese person in Wuhan, I am just as much a victim as someone here.”
He pointed out that many of the racist attacks are geared towards people who may find it difficult to defend themselves — the disenfranchised, immigrants or those who do not speak the language.
“It is going to be a single mom with three kids from China living in an impoverished area. And if they can’t defend themselves, then I have to use my platform to speak up against it,” Chiu said.
The Intensive Care Units (ICU) in most hospitals are currently at full capacity, leading to other floor units being transformed into ICU rooms. However, these rooms often do not receive the proper amount of attention due to the lack of resources or human capital.

Chiu said that vaccinations take at least a year to develop. According to the CDC, vaccines undergo three phases of clinical trials where the drug is tested on people for efficacy and safety. Many go through a fourth phase which involves ongoing studies even after the vaccine is approved and licensed.
But as the world waits on a vaccine, hospitals are beginning to face a crisis where the demand for care outweighs the hospital’s ability to do so.
“Now we are going into a phase where, sadly, we need to be selective in terms of how we provide intensive care. I hate to say it but I think we are starting to reach that stage,” he said.
Chiu anticipates the U.S. reaching its peak amount of cases within the next week or two. Then, eight to 10 weeks after that would be the beginning of taking “baby steps” back to normalcy. Essential businesses and outpatient centers will begin to open up, followed by transportation, and eventually restaurants and other businesses. However, there will still most likely be restrictions on non-essential businesses, according to Chiu.
“I think it will take longer than what most people would like to hear,” he said.
Chiu said the best way the public can help frontline healthcare practitioners is by mitigating the spread of the virus. That means taking social distancing very seriously and practicing good hygiene. Speaking against racism during this time, and recognizing workers at hospitals who are often underrepresented, can also help.
Dr. Jason Chiu has opened a new Facebook page, called ThePainlessDoc, where he will give periodic updates about the pandemic, posting recent statistics, and speaking about his personal experience working at the hospital during this time. He will also be providing consultation services where people can ask questions about the pandemic, and eventually, anything from how to prepare for surgery to pain mitigation after surgery.
Feature Images via Jason Chiu
The post Doctor Fighting on the Front Lines Reveals How a ‘Tiny Breathing Tube’ Separates Life and Death for Patients appeared first on NextShark.
Contributer : NextShark



 Reviewed by mimisabreena
on
Friday, April 10, 2020
Rating:
Reviewed by mimisabreena
on
Friday, April 10, 2020
Rating:















No comments:
Post a Comment